
An international team of researchers has discovered how cholesterol can disrupt the internal functioning of the heart by accumulating in the mitochondria of cardiomyocytes. They have also developed an experimental immunotherapy capable of reversing this process and restoring cellular energy production.
The study, recently published in the Journal of Lipid Research, was led by Dr. Vicenta Llorente-Cortés, researcher at the Lipids and Cardiovascular Pathology group of the Institute of Biomedical Research of Barcelona (IIBB-CSIC), part of the Spanish National Research Council (CSIC), the Sant Pau Biomedical Research Institute (IR Sant Pau), and the CIBERCV.
The research was conducted in collaboration with scientists from CIBERdem, the Institute of Molecular Biology of Barcelona (IBMB-CSIC), the University of Barcelona (UB), the Autonomous University of Barcelona (UAB), the University of California (USA), and the University of Toulouse (France).
The heart requires a high and constant energy supply and depends on the efficiency of its mitochondria to sustain continuous contraction of the cardiac muscle. In fact, cardiomyocytes (heart muscle cells) are among the most mitochondria-rich human cells—nearly a third of their volume consists of mitochondria. These organelles convert nutrients into energy through a process called oxidative phosphorylation, which is essential for heart function.
Several studies have indicated that under altered metabolic conditions—such as obesity, diabetes, or hypercholesterolemia—progressive mitochondrial dysfunction occurs, which worsens heart failure. This study identifies, for the first time, a precise cellular mechanism through which cholesterol esters, transported by lipoproteins, penetrate cardiomyocytes and accumulate inside their mitochondria, causing structural and functional impairments.
The researchers demonstrated that the LRP1 receptor, a protein located on the cell membrane of cardiomyocytes, is the main factor responsible for transporting esterified cholesterol from lipoproteins into cardiomyocytes. Under lipotoxic conditions, this cholesterol accumulates in mitochondrial membranes and interiors. The result is disruption of mitochondrial architecture, impairment of the respiratory chain, and a significant loss in energy production capacity.
“We have revealed a previously unknown mechanism: the cholesterol carried by lipoproteins doesn’t just affect blood vessels or accumulate in plaques—it actually penetrates the mitochondria of the heart. The accumulation of cholesterol esters in mitochondria compromises cellular respiration and, consequently, the function of the heart itself,” explains Dr. Vicenta Llorente-Cortés, CSIC researcher, lead author of the study, and coordinator of the CIBERCV and CIBERdem groups at IIBB-CSIC and IR Sant Pau.
To counter this harmful mechanism, the team developed an experimental immunotherapy based on monoclonal antibodies specifically targeting the P3 domain of the LRP1 receptor. This strategy achieves selective blockade that prevents the LRP1 receptor from transferring cholesterol esters—carried in the bloodstream by lipoproteins—into the cell interior.
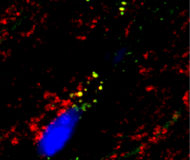
To conduct this research, the scientists used a combination of advanced bioenergetics techniques (University of California), mass spectrometry (University of Toulouse), and confocal and electron microscopy (IR Sant Pau and University of Barcelona). They used a rabbit model with a lipid profile similar to that of humans to simulate dyslipidemic conditions associated with cardiovascular disease (CSIC).
The researchers performed subcellular fractionation analyses to isolate mitochondria and quantify their lipid content, and used high-precision respirometry techniques to assess mitochondrial respiratory chain efficiency in the presence and absence of cholesterol accumulation in the hearts of the experimental model.
Trials conducted in the rabbit model—with a lipid and lipoprotein profile similar to that of humans—showed that this immunotherapy significantly reduces mitochondrial lipid load, particularly the content of cholesterol esters involved in cellular respiration. As a direct consequence, restoration of mitochondrial architecture was observed, including the recovery of mitochondrial aristae—key structures for cellular respiration. Furthermore, the therapy improves the efficiency of oxidative phosphorylation and normalizes ATP production, the energy molecule that powers heart contraction.
Another significant effect observed following treatment with anti-P3 antibodies was the improvement in the interaction dynamics between mitochondria and cytoplasmic lipid droplets, indicating a functional reorganization of cellular metabolism.
This therapeutic approach, both innovative and highly targeted, not only halts the damage caused by cholesterol accumulation but also reverses the effects on the heart’s energy machinery. According to the researchers, this strategy could potentially be applied in the future to treat various cardiovascular conditions where altered lipid profiles promote intracellular cholesterol deposition, such as in obesity, myocardial ischemia, or chronic hypercholesterolemia.
“Our experimental treatment allows us to act on the heart at a level that had not been targeted before: inside the cell, inside the mitochondria, where the vital energy of the cardiac muscle is generated,” emphasizes Dr. Vicenta Llorente-Cortés.
Cardiovascular diseases are responsible for one in three deaths worldwide. While current treatments have made significant advances in controlling traditional risk factors such as hypertension or plasma cholesterol, there is still no effective strategy to address intracellular metabolic damage in the heart, particularly mitochondrial damage.
This study proposes an entirely new approach: to intervene directly in the process that leads cholesterol to accumulate in the energy machinery of cardiac cells, thereby preventing the bioenergetic dysfunction that precedes heart failure.
“This discovery has clear clinical implications: it enables us to envision new therapies aimed at preserving mitochondrial function in patients with high cardiovascular risk. This is especially relevant in contexts where circulating cholesterol remains persistently elevated, and lowering it externally is no longer enough—we need to protect the heart from within,” concludes Dr. Llorente-Cortés.
This study was supported by the Carlos III Health Institute (ISCIII) through the cooperative research programs of the Biomedical Research Networking Centers in Cardiovascular Diseases (CIBERCV) and in Diabetes and Associated Metabolic Diseases (CIBERdem), as well as by funding from the European Regional Development Fund (ERDF). Additional funding came from the Spanish Ministry of Science, Innovation, and Universities, and from the Government of Catalonia through the Agency for Management of University and Research Grants (AGAUR). International collaborations were co-funded by research agencies in the United States and France, including the National Institutes of Health (NIH) and the Centre National de la Recherche Scientifique (CNRS).
Benitez-Amaro A, Garcia E, LaChica Lhoëst MT, Polishchuk A, Zegri-Reiriz I, Vilades D, Guerra JM, Fernández-Del-Rio L, Mirabet S, Samouillan V, Shirihai O, Liesa M, Enrich C, Llorente-Cortés V. LRP1 immunotherapy enhances cardiomyocyte respiration by restricting cholesteryl ester accumulation in mitochondria. J Lipid Res 2025:100783. https://doi.org/10.1016/j.jlr.2025.100783