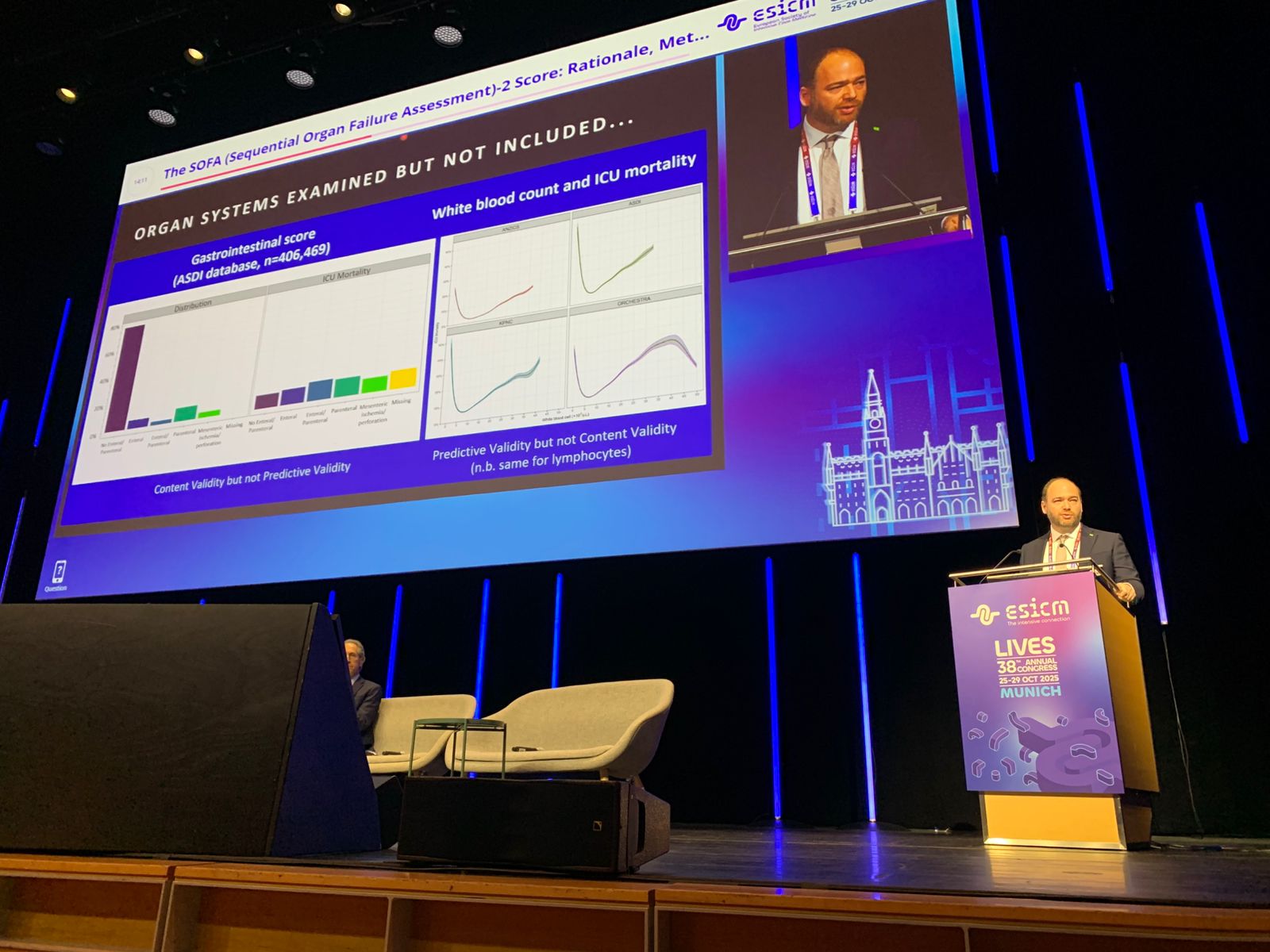
The Journal of the American Medical Association (JAMA) has recently published the updated version of the Sequential Organ Failure Assessment (SOFA), the global reference system in intensive care medicine used to assess the degree of organ dysfunction in critically ill patients. The results were also presented in parallel at the Annual Congress of the European Society of Intensive Care Medicine (ESICM LIVES 2025), held in Munich, in a featured session on current topics broadcast live.
SOFA-2, which replaces the model in place since 1996, incorporates advances in diagnostics, monitoring, and life support introduced over the past decades to more accurately reflect the reality of critically ill patients and the response of their organs to treatment.
The study was led by the international SOFA-2 Study Group consortium, with Dr. Otavio Ranzani, head of the Health DataLab at the Institut de Recerca Sant Pau (IR Sant Pau), serving as the leader of methodology and data analysis. The magnitude and diversity of the data analyzed—more than 3.3 million ICU admissions from nine countries—make this work the largest international review ever conducted on organ dysfunction measurement, setting a new benchmark for clinical practice and critical care research.
The SOFA system was conceived in 1994 and published in 1996 as a common language to describe dysfunction in six organs—brain, heart, lungs, liver, kidneys, and coagulation system—based on clinical and laboratory parameters. Since then, it has become an essential tool in both clinical practice and research, used to quantify the severity of critical illness.
Over the past three decades, intensive care has evolved profoundly. Today, clinicians have access to new monitoring devices, less invasive life-support therapies, and more specific drugs, as well as information systems that allow for a more dynamic and precise assessment of a patient’s condition. These advances made a complete update of the original model necessary.
“The way we treat patients in intensive care has changed enormously over the past three decades,” explains Dr. Otavio Ranzani, first author of the study. “We now have noninvasive ventilation, continuous renal replacement therapies, and circulatory support with much more precise devices and drugs. The SOFA system needed to reflect that reality so we can better describe organ dysfunction and compare patient severity consistently across the world.”
SOFA-2 maintains the structure of six organ systems but redefines the scoring thresholds and updates the variables used. Key innovations include the addition of extracorporeal membrane oxygenation (ECMO) and high-flow oxygen therapy in the respiratory component, a new classification for vasopressor dosing in the cardiovascular component, and revised criteria for assessing liver, kidney, and coagulation function. The new model achieves a more uniform gradation of severity and a tighter relationship between score and clinical outcomes.
The SOFA update was conducted in eight stages, combining expert consensus with large-scale clinical data analysis. First, a Delphi process brought together 60 international specialists from 25 countries, including two from Spain—Dr. Otavio Ranzani and Dr. Ricard Ferrer from Vall d’Hebron University Hospital—who reached consensus on the conceptual principles and key variables of the new model. The research team then validated these proposals using advanced statistical analyses across ten national registries of critically ill patients, totaling more than 3.3 million ICU admissions from Australia, Austria, Brazil, France, Italy, Japan, Nepal, New Zealand, and the United States, thus encompassing diverse healthcare systems and resource levels across four continents.
The result is a system that preserves the simplicity of the original SOFA while providing a much stronger empirical foundation and revised clinical criteria based on the analysis of millions of real-world cases. Each point on the scale was calibrated to correspond to a progressive and clinically consistent increase in mortality risk, validated across different cohorts and countries. Additionally, detailed instructions for data collection and interpretation were incorporated, ensuring uniform application across various care settings. Altogether, SOFA-2 provides a more accurate and contemporary representation of critical care management in the 21st century while maintaining the clarity and ease of use that characterized the original model.
“SOFA-2 is the result of an unprecedented scientific consensus in intensive care medicine,” emphasizes Dr. Ranzani. “It integrates the best available evidence with the accumulated clinical experience from highly diverse settings—from high-complexity university hospitals to resource-limited units. This ensures that the tool is truly global.” The results confirmed that SOFA-2 more accurately describes the progression of vital organ function in critically ill patients, showing a highly consistent relationship between score and observed mortality.
Beyond its statistical performance, the main contribution of SOFA-2 lies in its greater clinical applicability. The new model accounts for the realities of hospitals with varying resource levels and defines clear rules for data recording and interpretation, reducing variability between units and countries.
“We wanted SOFA-2 to be useful both in a large European hospital and in an ICU in a developing country,” notes Dr. Ranzani. “Our goal was to provide a standardized, up-to-date, and global tool to support both research and clinical decision-making.”
The system also improves consistency in intermediate levels of dysfunction, avoiding abrupt jumps between categories and allowing for a more intuitive gradation of organ deterioration. This enhances its value for daily clinical monitoring and for comparing outcomes across institutions or therapeutic trials. Moreover, it includes instructions adapted to resource-limited settings, enabling reliable use even in environments where certain treatments or measurements are unavailable.
Another key contribution of SOFA-2 is its ability to harmonize intensive care research. By incorporating globally applicable and updated criteria, SOFA-2 facilitates comparison across multicenter studies and improves the quality of clinical trials. This methodological uniformity is essential for advancing toward a more data-driven and internationally valid field of intensive care medicine.
Researchers also highlight its usefulness for monitoring quality of care in ICUs, as it provides a sensitive and standardized indicator of organ dysfunction among treated patients. The team considers this update a turning point in how critical illness is quantified, offering a more precise, dynamic, and practice-aligned framework.
“SOFA-2 is a long-awaited update that enhances intensive care medicine’s ability to measure, understand, and treat critical illness,” concludes Dr. Otavio Ranzani. “By more faithfully reflecting patients’ physiology and the interventions they receive, this new system will enable better evaluation of treatment effects and support progress toward more personalized and efficient care.”
You can listen to this podcast in English about the publication.
And here’s a video on Instagram.
Ranzani OT, Singer M, Salluh JIF, et al. Development and Validation of the Sequential Organ Failure Assessment (SOFA)-2 Score. JAMA. Published online October 29, 2025. doi:10.1001/jama.2025.20516
Last update: 17 de November de 2025